The U.S. Preventive Services Task Force (USPSTF) recently changed its recommendations for all women to get screened for breast cancer every other year starting at age 40 instead of 50.
Wanda Nicholson, USPSTF Vice Chair and professor at George Washington University said the updated recommendations “will save more lives among all women.”
Sadly, it’s not that simple.
Time and time again, the evidence shows that screening healthy women using mammograms in fact, does not save lives.
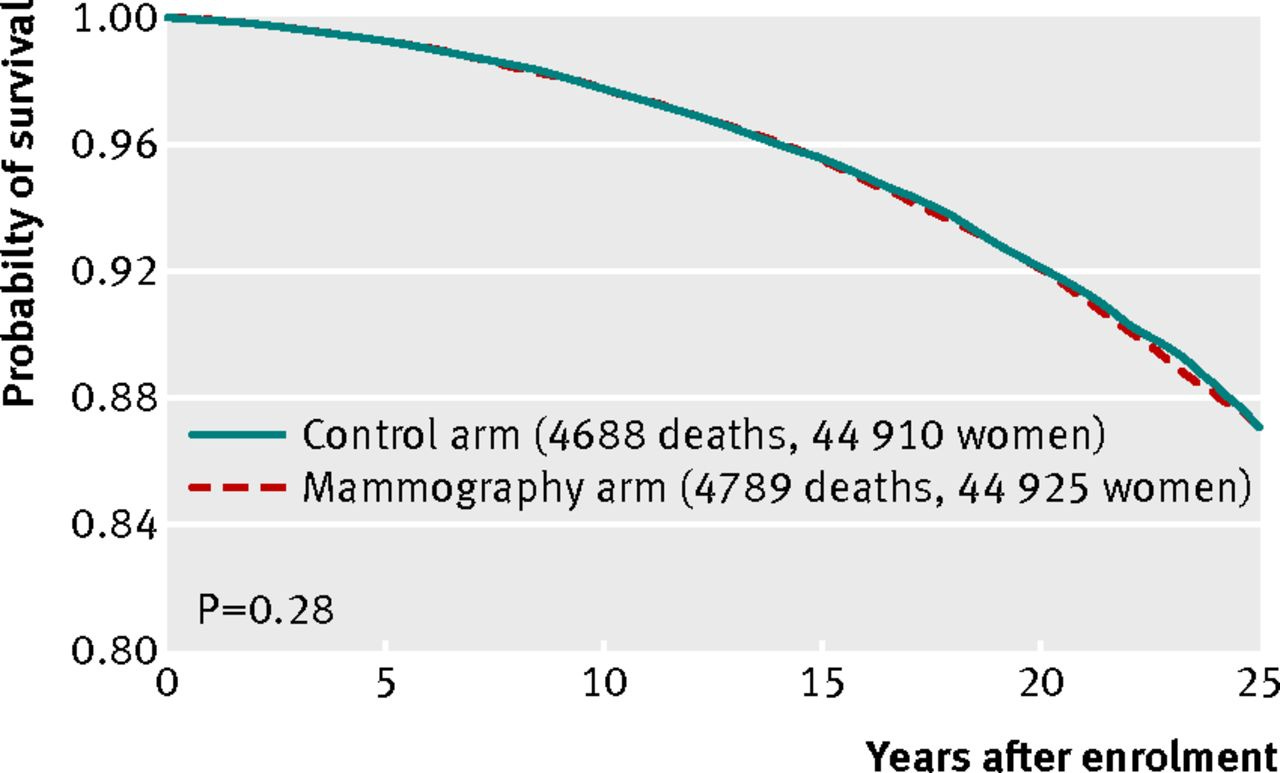
In 2014, in a large study published in The BMJ, half of women underwent annual mammogram screening, and the other half did not.
At the end of the 5-year trial period, and after 25 years of follow-up (see graph), the probability of survival was similar in the two groups.
A Cochrane review in 2013 (and an unpublished update in Jan 2023) also found mammography screening had no impact on the most important outcome, i.e. overall (all-cause) mortality.
How is it possible that detecting cancers earlier doesn’t save lives?
The imaging technology is so sensitive that it detects lumps, masses and cysts that are not cancerous, resulting in biopsies and follow-up procedures that can cause patients immense stress.
Also, it’s detecting abnormalities that would never lead to harm because they grow so slowly, or they don’t grow at all.
And because we’re not very good at distinguishing the difference between slow and fast-growing cancers, the standard is to treat them all – sometimes, unnecessarily.
Danish physician Peter Gøtzsche and lead author of the Cochrane review on mammography screening wrote a review in 2015 called “Mammography screening is harmful and should be abandoned.”
Gøtzsche explains why screening healthy women actually harms more than it helps. It’s a well-intentioned program that has unintended harmful consequences.
For example, while trying to reduce death from breast cancer, the treatments (e.g. radiotherapy) may cause death from other diseases like heart disease or lung cancer - so in the end - there is no improvement in lifespan.
Much of the difficulty lies with ~20% of breast abnormalities called “Ductal Carcinoma In Situ (DCIS) – otherwise known as stage 0 cancer. Their detection is a direct consequence of the mammography screening, as they would not be detected otherwise.
Importantly, these are not cancers, but have the potential to progress.
The problem is, few clinicians are comfortable with the wait-and-see approach, and often encourage women to undergo invasive surgeries, radiation, or chemotherapy that they didn’t ultimately need.
For this reason, some oncologists have suggested changing the name of DCIS to avoid using words such as “stage 0 cancer” or “carcinoma” which cause fear and unnecessary psychological stress.
The question of whether patients benefit from immediate treatment of DCIS or from ‘active surveillance’, may be answered over the next few years by three ongoing trials – two in Europe and one in the US.
Too Much Medicine
Lowering the screening threshold from age 50 to 40, means millions more people become eligible for treatments that they might not need, under the guise of “prevention is better than cure.”
Consequently, a huge number of scarce resources is diverted from the sick to the ‘worried well.’
Dr Iona Heath, past president of the UK Royal College of General Practitioners, once said to me, “Medicine should probably be leaving the well to be well, instead of constantly trying to find something wrong with them.”
Dr Heath was among several experts who featured in my documentary called “Too Much Medicine” which aired on ABC TV in 2015 (see above). The program explored the issue of over-diagnosis and over-treatment in various areas of healthcare.
There are women at high risk of breast cancer - e.g. those with a genetic/family history – who might benefit from targeted detection tools, but screening women in the general population appears to cause more harm than good.
*15 of the 16 members of the US Task Force declared no conflicts of interest related to this recommendation. There was only one Task Force member who had a relevant conflict of interest, and he was recused from all activities related to this recommendation.
*Peter Gøtzsche, former head of the Nordic Cochrane Centre, published a book titled “Mammography Screening: Truth, Lies and Controversy” available here.
*Vinay Prasad, a practicing haematologist-oncologist and Professor in the Department of Epidemiology and Biostatistics at the University of California San Francisco, has recently produced a video explaining the data.







Mammograms for women 40 & over?